Four years into the pandemic, my refusal to align myself with the rest of society sleepwalking into a replay of 2019 norms of work and life has set me back for years personally and professionally. Many parties are trying to hoodwink the public into thinking that the pandemic is over in pursuit of short-term economic gain, while practically ensuring long-term economic and health catastrophe across the globe. Despite policymakers, public intellectuals and journalists’ attempt to wish the pandemic away, the Covid-19 pandemic remains, in 2024, a clear and present danger to public health.
Not the post-Covid you’re thinking of
While the public health emergency may have sunset, what has not is how 2020 marked a pivotal turning point in the science of disease transmission. Concerns about the air extend to more than just covid. Every pathogen that can transmit through air droplets is implicated, including rapidly spreading pathogens like measles and future novel airborne pathogens.
Early on in the pandemic, aerosol engineer Lindsey Marr wondered why a January 2020 article in the New York Times communicated that coronaviruses travelled shorter distances than viruses like measles, when her prior work on the flu virus suggested that SARS-Cov2 should be treated like any other airborne pollutant. Subsequent research about airborne transmission provided an explanation for bizarre superspreader events that couldn’t be explained by the widely accepted idea that surface transmission was the dominant route for transmission of diseases like covid-19, such as how covid-19 could spread across a room despite the then-accepted idea that airborne droplets travel no more than 2 metres.
The simple implication of the science of airborne pathogens tells us is that in a ‘post-Covid’ society, the air must be cleaned Unlike vaccines, cleaning the air is a variant-proof solution. Moreover, there are clear co-benefits of cleaning the air: a worldwide study reveals that short-term exposure to fine particulate matter (PM2.5) contributes to roughly 1 million premature deaths annually. I am fortunate to be in Asian society where people have generally fallen in line with the use of high-quality masks even-as vital protection against disease, but it’s anyone’s guess how long it’ll last.
No thanks to incoherent public health messaging, societal norms do not reflect any understanding of the airborne route of disease transmission, from masks off for photos to indoor meals, and now with everyone ‘forgetting’ Covid-19, masks off altogether. At the height of the pandemic, the WHO and other public health agencies have consistently failed to acknowledge the prominence of the airborne route for transmission of SARS-Cov2. Up until very recently, local and international health agencies have consistently placed recommendations for hand hygiene above air hygiene measures in public health communication.
To the credit of the public health authorities, there has been a quiet shift in their position on the importance of cleaning indoor air. The new CDC recommendations stress the importance of air filtration and ventilation, and as early as 2021 Malaysia’s DOSH has issued air quality guidelines for commercial and residential settings. Yet thanks to public health authorities dragging their feet on acknowledging the science at the height of the pandemic, people have abdicated their responsibilities to mitigate airborne infection altogether, resulting in fundamentally unsafe public spaces. Consequently, health authorities in the US have watered down recommendations to align with what society can accept, even when the science dictates otherwise.
Even though novel solutions such as UV-C and C-R boxes have been developed to complement HEPA filters and other solutions, the general public has been hoodwinked into thinking that nothing can and should be done to reduce disease transmission.
Multi-system consequences
The pandemic thus far has been devastating to humanity. The Economist estimated the toll of the pandemic to be 35mil up to March 2024, just over Malaysia’s total population. Estimates of life expectancy suggest that Covid-19 has resulted in a loss of life expectancy at birth of 1.6 years, the largest drop since the Second World War. The costs of the pandemic, however, stretch far beyond mortality. The narrow framing of the health consequences of Covid-19 in terms of hospitalisations and deaths has led policymakers to ignore the chronic phase of Covid disease, colloquially known as Long Covid.
Long Covid parallels Nassim Taleb’s description of ‘black-swan events’: low-likelihood, high-impact situations that are not often incorporated in people’s risk calculus. However, absent mitigation, the chances of contracting Long Covid would certainly not qualify as a black swan event. Estimates of the incidence of long-term complications from Covid infection range from 10-50% per infection. Moreover, Covid-19 isn’t subject to the same seasonality as the flu, with people contracting 2-3 infections a year.
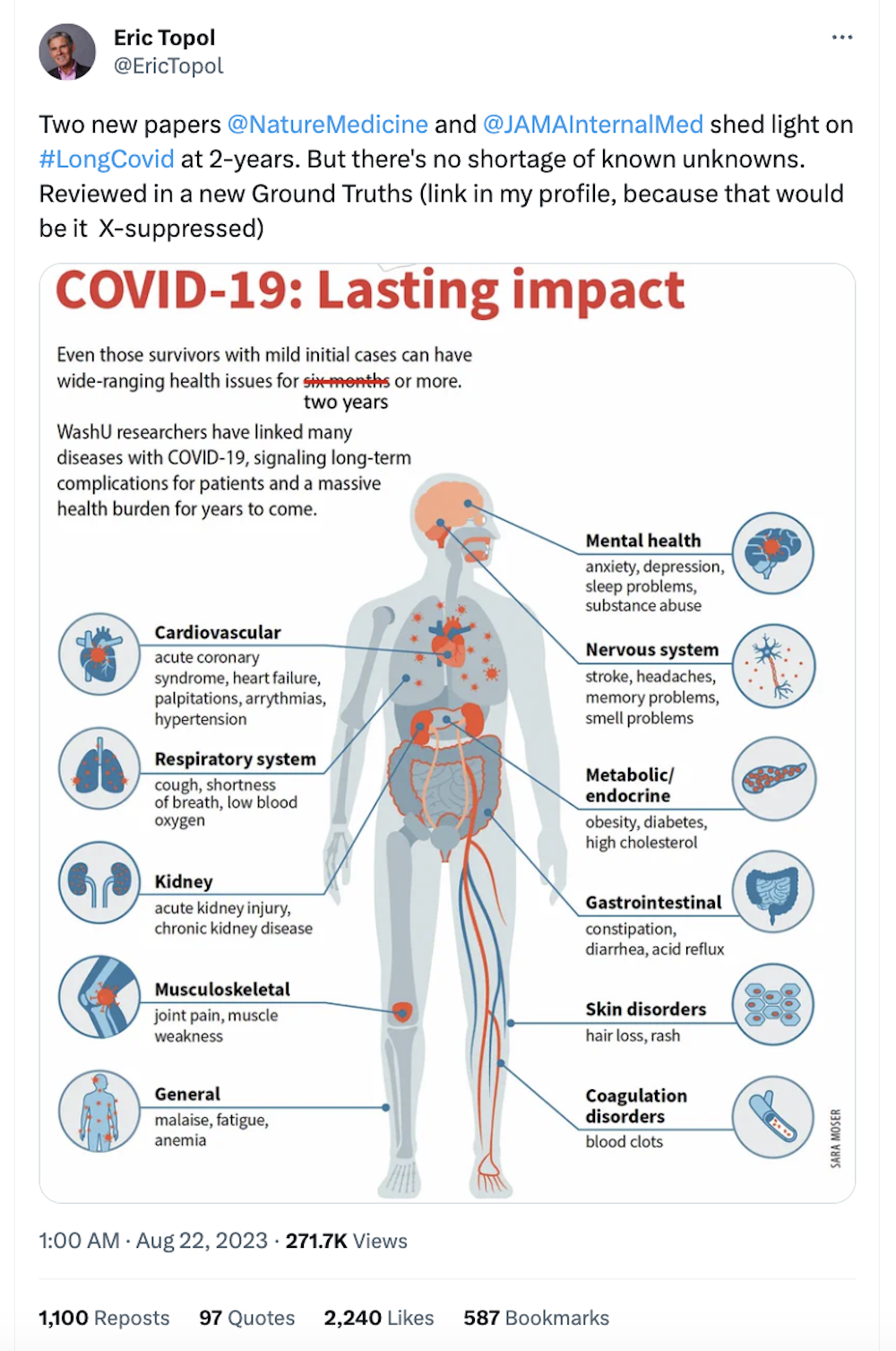
Much has been documented about the consequences suffered by Long Covid patients, some of them who may have contracted Covid despite not exhibiting symptoms. There is no known cure for the disease. Some experts describe Covid as “not a disease of the lungs at all” but rather a “vascular and neurologic infection”. Moreover, the cognitive consequences of Long Covid are striking, equivalent to 10 years of aging. It is bizarre that Covid-19 isn’t treated as a serious occupational hazard. Rather, the consequences are so dire and rampant, a Californian court opined that were it to be treated as the occupational hazard that it is, the court would be brought to a standstill. Health issues that have classically been understood as non-communicable diseases are now literally airborne, yet the consequences of that have barely registered among policymakers.
David Cutler published estimates of the economic cost of Long Covid at 3.7 trillion USD, or 17% of 2019 US GDP. In an online forum organised by a US-based insurer, he expressed that the magnitude of the problem is such that there is no amount of investment towards preventing and curing Long Covid that would not be worth it. Young people stand to lose the most from Long Covid with more life-years, children are not spared, with estimates suggesting some 5.8 million children in the US suffer from Long Covid.
Increased threat level
Vaccines play a vital role in reducing the incidence of Covid-19 infection, severe disease and death. however they do not prevent infection completely. Moreover, considering the rapid evolution of covid-19 and especially the lack of available updated vaccines in our part of the world, calling for covid-19 precautions to be lifted is beyond premature. It has been established that vaccine-induced immunity to Covid-19 drops sharply in less than a year, and it should be clear that vaccine-acquired immunity is much safer than infection-acquired immunity.
Some reassure us that we are not in 2021. We certainly are not: vaccines have not kept pace with the rapid mutation of Sars-Cov2. Malaysia has only had access to vaccines based on the 2020 strain of the virus thus far. Availability of current vaccines is limited.
Despite this, society has been lulled into a false sense of security powered by groupthink. But groupthink logic is counterproductive in an active pandemic: when less people take precautions that reduce the risk for other people, the higher the risk for everyone else. Complacency about airborne pathogens is widespread amid the complete abdication of airborne disease mitigations. Generations to come will suffer for public intellectuals and politicians’ willful ignorance to avoid footing the costs of the practical and sensible normalisation of air filtration and ventilation measures.
The WFH no-brainer
Despite the established science on airborne disease transmission, employers insist that employees infect each other with any variety of airborne pathogen anywhere from 3 to 5 days a week, on top of denying medical leave for Covid. To add insult to injury, thought leaders continue to normalise in-person, unmasked superspreader events, accelerating the spread and mutations of and beyond covid-19, without regard for how in-person events exclude geographically distinct communities from vital policy conversations.
RTO in an active pandemic is a marker of the devaluation of knowledge work: knowledge workers are being infantalised when employers tell them that they have to come in the office to be productive. It is no wonder that there’s barely a squeak about the knowledge economy, when the implied consensus of the public’s nihilistic approach to Covid is that cognitive ability no longer matters.
In addition to the potential to inflict long-term loss of health and life, the accelerating and looming threat of climate change makes it reckless to engage in activities that involve substantial, repeated travel considering the urgency of de-escalating emissions. WFH has been shown to cut over half of carbon emissions relative to in-person work, and that doesn’t even include carbon-intensive work flights that could be conducted over an hour-long Zoom meeting. Thought leaders feign ignorance of how surface temperature records have been broken for each of the past 12 months, even as researchers continue to be stunned by ocean temperature measurements.